Ebola: a study in Guinea reveals persistent immunity five years after vaccination
 |
 |
Paris, le 5 septembre 2024
Press information
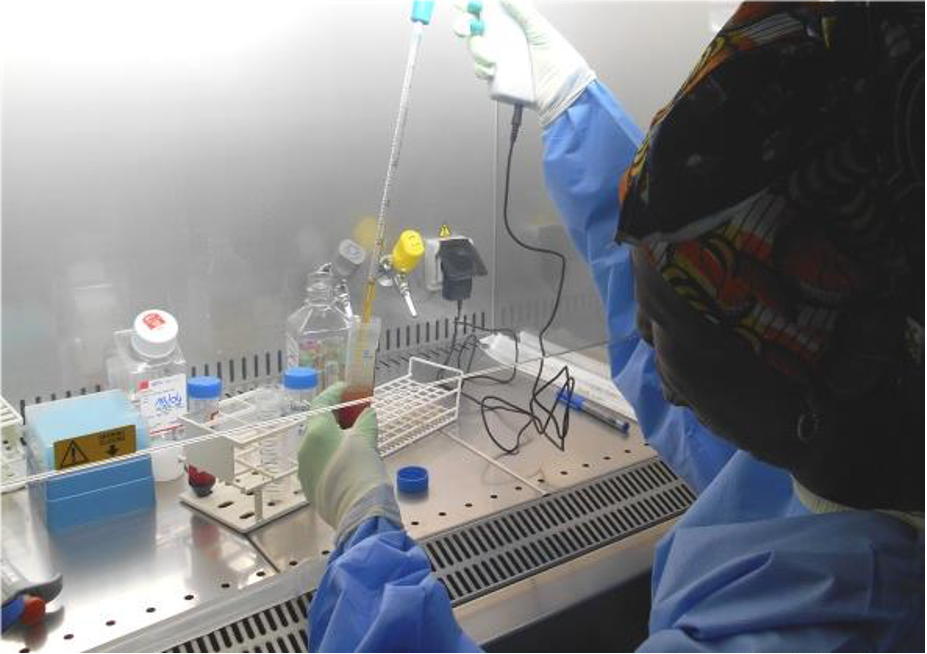
© Aurélie Wiedemann
Epidemics of Ebola virus disease occur periodically in several sub-Saharan African countries. Two vaccines have already received WHO prequalification against the Ebolavirus Zaire species. However, information on the long-term immune response to these vaccines is still insufficient. We need to consolidate our knowledge on this subject to continue developing the safest and most effective vaccination strategies possible, for both adults and children. In a new study conducted in Guinea, scientists from VRI, Inserm and Université Paris-Est Créteil (U955 Institut Mondor de recherche biomédicale) have taken a further step in this direction. They have shown that the cellular immune response induced by three different vaccine strategies is maintained for up to five years after vaccination. These results, which support current vaccine strategies against Ebola, are published in Nature Communications.
The Ebola virus causes high fevers and hemorrhages, often resulting in death. Many countries in sub-Saharan Africa regularly face epidemic outbreaks. the Ebola virus caused the largest epidemic known to date in West Africa in 2014. It has since re-emerged several times in the DRC, but also in Guinea. Vaccination is today one of the most effective tools for combating the disease, and one of the major challenges for research and public health strategy is to continue improving knowledge of the immune response induced in the long term by currently available vaccines.
Since 2019, two vaccines have obtained WHO prequalification against the Ebolavirus Zaire strain: the rVSVΔG-ZEBOV-GP vaccine (Ervebo®), developed by Merck, Sharpe & Dohme, Corp. and the vaccine regimen comprising Johnson & Johnson’s Ad26.ZEBOV (Zabdeno®) vaccine and Bavarian Nordic’s MVA-BN-Filo (Mvabea®) vaccine.
In 2022, the international PREVAC consortium (see box at the end), comprising Inserm, NIH and the London School of Hygiene and Tropical Medicine (LSHTM), published a study in the New England Journal of Medicine examining the safety and efficacy of three vaccine regimens:
• The first vaccine regimen tested consisted of one dose of Ad26.ZEBOV vaccine, followed 56 days later by one dose of MVA-BN-Filo;
• The second regimen involved a dose of rVSVΔG-ZEBOV-GP;
• Finally, the third schedule began with a dose of rVSVΔG-ZEBOV-GP, followed 56 days later by a booster dose of the same vaccine.
Published results showed a high serum antibody response 12 months after vaccination. However, it was essential to obtain information on the long-term maintenance of the response, and in particular regarding the cellular response (see box below).
| Humoral response and cellular response
Adaptive immune responses fall into two broad categories: the humoral response, based on the production of antibodies, by B lymphocytes, that recognize and neutralize the virus before it infects cells, and the cellular response, where CD8+ T lymphocytes identify and destroy already-infected cells to limit the spread of the virus. CD4+ T lymphocytes play a crucial role in helping B lymphocytes produce antibodies, boosting the effectiveness of the immune response. |
In December 2023, the 5-year follow-up of participants in the PREVAC clinical trial was completed. The results are being analyzed and will enable assessment of long-term immunity. sIn an ancillary study, scientists analyzed cellular immunity in 230 participants in Guinea, just after vaccination, at one year and five years post-vaccination.
“This is the first study from the PREVAC consortium to look specifically at participants’ cellular immune response. It completes the knowledge already acquired on the humoral response at one year and offers the first follow-up results at 5 years”, emphasizes Aurélie Wiedemann, immunologist at VRI and the Institut Mondor de recherche biomédicale (Inserm/Université Paris Est Créteil) and first author of the study.
Using blood samples taken in Conakry, the scientists were able to analyze the response of CD4+ and CD8+ T lymphocytes to vaccination. They showed the presence of anti-Ebola CD4+ T cells five years after vaccination, regardless of the vaccination regimen. The persistence of these responses is important for the maintenance of humoral immune memory in the event of exposure to the Ebola virus. In a subgroup of volunteers, the authors show a correlation between CD4+ T cell response and the quantity of specific antibodies in the long term.
While CD4+ T response is important for maintaining an antibody response, the presence of cytotoxic CD8+ T cells is also crucial for effective antiviral protection. A specific CD8+ T cell response was demonstrated in individuals vaccinated with two of the three vaccine regimens.
“These results will shortly be supplemented by humoral response data – on antibody production – from all PREVAC consortium countries, on a larger number of participants. Nevertheless, these results are promising and suggest that vaccination against the Ebola virus can induce long lasting immunity. They also pave the way for adjusting current vaccination strategies, by making it possible to assess, for example, the need for a long-term booster vaccination”, explains Prof. Yves Lévy, Director of the VRI and final author of the study.
In 2020, the team also published a study in Nature Communications on the immunity of Ebola survivors two years after discharge from hospital. One of the next avenues of research could be to compare the long-term immune response of these survivors with that induced by vaccination, in order to identify possible correlates of protection against infection, as these are currently undetermined.
Thus, this new study could help identify vaccine responses that would be effective against the infection, improve current vaccine strategies, and define long-term booster vaccine strategies to maintain protection for particularly at-risk individuals such as healthcare workers in Africa.
| About PREVAC
PREVAC (Partnership for Research on Ebola Vaccinations; NCT02876328) is an international consortium conducting researches in West Africa to evaluate the safety and efficacy of Ebola vaccination. |
Notes
-
1. Prequalification means that a vaccine meets WHO standards of quality, safety and efficacy. On the basis of this recommendation, UN agencies and the Gavi Alliance can purchase the vaccine for at-risk countries.
-
2. This analysis was carried out in collaboration with the SISTM team at the Bordeaux Population Health Research Center (UMR 1219 Université de Bordeaux/Inserm).
-
3. These are immunological markers associated with protection against infection: for example, post-vaccination antibody levels against hepatitis B are a good correlate of protection. In other words, in the context of vaccination, they designate the parameters that scientists monitor to find out whether the vaccine works and protects effectively against infection.
Sources
Long-term cellular immunity of vaccines for Zaire Ebola Virus Diseases
Aurélie Wiedemann1,2¥, Edouard Lhomme1,3,4¥ Mélanie Huchon1,4, Emile Foucat1,2, Marion Bérerd-Camara5, Lydia Guillaumat1,2, Marcel Yaradouno5, Jacqueline Tambalou5, Cécile Rodrigues1,2, Alexandre Ribeiro1,2, Abdoul Habib Béavogui6, Christine Lacabaratz1,2, Rodolphe Thiébaut1,3,4, Laura Richert1,3,4, Yves Lévy1,2,7*, and the Prevac study teama
1. Vaccine Research Institute, Université Paris-Est Créteil, France
2. INSERM U955, Institut Mondor de Recherche Biomedicale (IMRB), Team Lévy, Créteil, France
3. Univ. Bordeaux, INSERM, Institut Bergonié, CHU de Bordeaux, CIC-EC 1401, Euclid/F-CRIN clinical trials platform, Bordeaux, France
4. Univ. Bordeaux, Inserm, Population Health Research Center, UMR 1219, INRIA SISTM, Bordeaux, France
5. Alliance for International Medical Action
6. Centre National de Formation et de Recherche en Santé Rurale (CNFRSR), Maferinyah, Guinea
7. Assistance Publique-Hôpitaux de Paris, Groupe Henri-Mondor Albert-Chenevier, Service Immunologie Clinique, Créteil, France
Researcher contact
Yves Lévy
Institut Mondor de Recherche Biomédicale (U955 Inserm/Université Paris-Est Créteil)
Vaccine Research Institute (VRI)
E-mail : yves.levy@inserm.fr
Aurélie Wiedemann
Institut Mondor de Recherche Biomédicale (U955 Inserm/Université Paris-Est Créteil)
Vaccine Research Institute (VRI)
E-mail : aurelie.wiedemann@inserm.fr
Téléphones sur demande
Contact presse
presse@inserm.fr
Accéder à la salle de presse de l’Inserm